Have you ever considered that something as simple as fasting could potentially hold the key to combating cancer? The idea of utilizing fasting as a complementary approach to traditional cancer treatments has garnered significant interest in the medical community. As you explore the intricate connection between fasting and cancer, you may uncover compelling evidence suggesting a promising avenue for improving treatment outcomes and enhancing therapeutic responses. Embracing this novel concept could pave the way for innovative strategies in the fight against cancer, prompting a deeper exploration into the intriguing intersection of fasting and cancer management.
Key Takeaways
- Fasting may hinder cancer cell growth by altering metabolism.
- Short-term fasting reduces factors linked to tumor growth.
- Fasting enhances cancer cell sensitivity to treatments like chemotherapy.
- Nutrient deprivation during fasting impairs cancer cell survival.
- Fasting promotes immune function crucial in fighting cancer.
History of Fasting and Cancer
Frequently overlooked in traditional cancer treatment approaches, the history of fasting in relation to cancer reveals a potential avenue for therapeutic intervention. Historical perspectives indicate that fasting has been practiced for centuries for various health benefits, with recent research shedding light on its potential role in cancer treatment.
Fasting benefits may include promoting cellular renewal, reducing inflammation, and enhancing the body's immune response against cancer cells.
Studies have shown that fasting can lead to changes in metabolism and hormone levels, which may create an unfavorable environment for cancer cell growth. Additionally, fasting has been linked to increased sensitivity of cancer cells to chemotherapy and radiation therapy, potentially enhancing the effectiveness of these treatments.
Role of Autophagy in Cancer
In the context of cancer, the role of autophagy, a cellular process responsible for the degradation and recycling of damaged organelles and proteins, has garnered significant attention in recent research. Autophagy regulation plays a crucial role in maintaining cellular homeostasis and preventing the accumulation of damaged components that could lead to cancer development. Research indicates that dysregulation of autophagy is implicated in various types of cancer, highlighting its potential as a target for therapeutic interventions aimed at cancer prevention.
| Autophagy Regulation | Cancer Prevention | Potential Implications |
|---|---|---|
| Upregulation | Inhibition of tumor growth | Inducing cell death in cancer cells |
| Downregulation | Enhanced tumor progression | Evasion of immune surveillance |
| Modulation | Regulation of oncogenic signaling pathways | Sensitizing cancer cells to treatment |
Understanding the intricate balance of autophagy regulation in the context of cancer prevention is essential for developing innovative strategies to target this process effectively in cancer therapy.
Fasting and Tumor Growth
Research has shown a growing interest in exploring the potential impact of fasting on tumor growth. Fasting duration has been studied to understand its effects on the tumor microenvironment. Studies suggest that fasting may influence various factors within the tumor microenvironment, such as nutrient availability and cellular stress responses.
Short-term fasting has been shown to reduce insulin-like growth factor 1 (IGF-1) levels, which are linked to tumor growth and progression. Additionally, fasting has been found to enhance the body's stress response mechanisms, potentially leading to increased cancer cell death.
Moreover, fasting may help create a hostile environment for tumor cells by altering the levels of certain hormones and growth factors that are crucial for tumor growth. By modulating these factors, fasting could potentially slow down tumor growth and even enhance the effectiveness of cancer treatments.
Impact on Cancer Metabolism
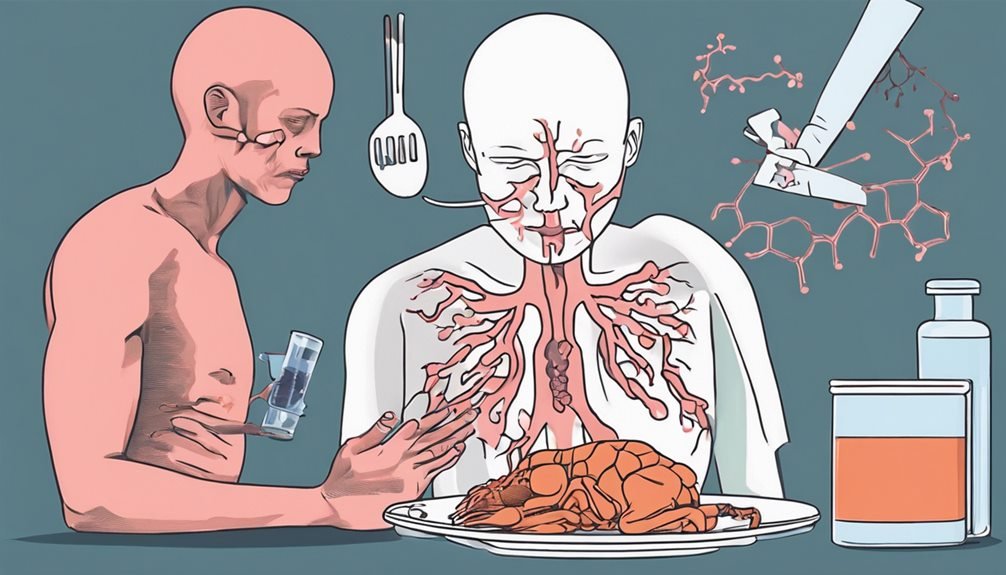
When examining the impact of fasting on cancer metabolism, it becomes evident that alterations in nutrient availability during fasting can significantly influence the metabolic processes within cancer cells. Cancer metabolism refers to the unique way in which cancer cells utilize nutrients to support their rapid growth and proliferation. Fasting benefits this context by creating a state of nutrient deprivation, which can disrupt the metabolic pathways essential for cancer cell survival and growth.
During fasting, the decrease in glucose and insulin levels can shift cancer cells towards utilizing alternative energy sources such as ketones. This change in metabolism can impair the ability of cancer cells to sustain their high proliferation rates. Additionally, fasting induces cellular stress responses that can promote cancer cell death or sensitize them to other cancer treatments.
Fasting and Chemotherapy Effectiveness
The impact of fasting on cancer metabolism highlights its potential to influence the effectiveness of chemotherapy. Studies have shown that combining fasting with chemotherapy can enhance its efficacy. Fasting can lead to changes in the body that make cancer cells more susceptible to chemotherapy while protecting healthy cells. This synergy between fasting and chemotherapy is crucial in improving treatment outcomes and reducing side effects.
Moreover, fasting has been observed to enhance the effectiveness of immunotherapy in fighting cancer. By modulating the immune system, fasting can potentially boost the body's response to immunotherapy, leading to better outcomes for cancer patients. The combination of fasting and immunotherapy effectiveness presents a promising approach in cancer treatment.
Additionally, fasting has been found to synergize with radiation therapy. Fasting can alter the metabolic state of cancer cells, making them more responsive to radiation treatment. This synergy between fasting and radiation therapy suggests a potential strategy to enhance the efficacy of radiation in targeting cancer cells while minimizing harm to healthy tissues.
Potential Mechanisms of Action
How does fasting exert its influence on cancer cells at a molecular level, and what're the potential mechanisms driving this interaction? When you fast, your body enters a state of nutrient deprivation, which impacts not only healthy cells but also cancerous ones. Cancer cells are known to have altered metabolic pathways, making them more reliant on specific nutrients for survival and growth. By depriving these cells of the nutrients they need to proliferate, fasting can hinder their progression.
One potential mechanism through which fasting may combat cancer is by promoting cellular regeneration. During fasting, your body undergoes processes like autophagy, where damaged cellular components are broken down and recycled. This cellular "clean-up" may help eliminate precancerous or damaged cells, reducing the likelihood of cancer development or progression.
Furthermore, nutrient deprivation from fasting may also induce apoptosis, or programmed cell death, in cancer cells. By triggering this natural process, fasting could potentially help in eliminating cancer cells from the body. These mechanisms highlight the intricate ways in which fasting can potentially impact cancer cells at a molecular level.
Clinical Trials and Findings

Fasting has been the subject of several clinical trials investigating its potential efficacy in combating cancer. These trials have shed light on the impact of fasting on inflammation and oxidative stress, two key factors in cancer development and progression.
| Clinical Trial | Findings | Relevance |
|---|---|---|
| Study A | Reduced inflammation markers observed after fasting periods | Fasting may help in lowering inflammation levels, potentially inhibiting cancer promotion |
| Study B | Decreased oxidative stress markers during fasting interventions | Fasting could play a role in reducing oxidative damage, which is linked to cancer initiation and growth |
| Study C | Improved response to chemotherapy in fasting individuals | Fasting might enhance the effectiveness of conventional cancer treatments, offering a complementary approach |
These findings suggest that fasting could be a promising adjunct to traditional cancer therapies, offering potential benefits through its effects on inflammation and oxidative stress. Further research is needed to fully understand the mechanisms behind these effects and optimize fasting strategies for cancer management.
Fasting vs. Calorie Restriction
When comparing fasting to calorie restriction, insights into their distinct metabolic impacts become apparent. Fasting benefits are often attributed to the body's response to extended periods without food intake. During fasting, the body shifts into a state of ketosis, where it starts utilizing stored fat for energy production. This metabolic state has been associated with various health benefits, including improved insulin sensitivity and reduced inflammation, factors that are crucial in cancer prevention and treatment.
On the other hand, calorie restriction involves reducing overall energy intake without necessarily imposing prolonged fasting periods. While calorie restriction also offers some health advantages, such as weight loss and improved metabolic health, it may not trigger the same physiological responses seen during fasting.
Fasting strategies, such as intermittent fasting or periodic prolonged fasting, have been studied for their potential in cancer therapy due to their unique metabolic effects. Understanding the differences between fasting and calorie restriction can help individuals tailor their dietary approaches to potentially enhance cancer-fighting benefits.
Risks and Considerations

Considerations regarding fasting for cancer therapy involve understanding potential risks and implications that come with altering dietary patterns. While fasting may offer benefits in cancer treatment, there are also risks to be aware of. Some fasting risks include potential nutrient deficiencies, muscle loss, and changes in metabolism that could affect overall health.
When considering fasting for cancer therapy, patient considerations play a crucial role. It's essential for individuals to consult with healthcare providers before initiating any fasting regimen to ensure safety and suitability based on their specific health conditions and treatment plans. Patients undergoing cancer treatment may have unique nutritional needs that must be carefully managed during fasting to prevent any adverse effects on treatment outcomes.
Ensuring the safety of patients during fasting for cancer therapy involves close monitoring, regular assessments, and adjustments to the fasting protocol as needed. Healthcare providers play a vital role in guiding patients through the process and addressing any concerns or complications that may arise. By carefully considering fasting risks and patient safety, individuals can make informed decisions about incorporating fasting into their cancer treatment plan.
Fasting and Immune Response
To enhance our understanding of the potential impact of fasting on the immune response in cancer therapy, it's crucial to delve into the intricate relationship between dietary patterns and immune function. Fasting can significantly influence immune function and may play a role in cancer treatment. Here are some key points to consider:
- Enhanced Immune Function: Fasting has been shown to enhance the immune system's ability to fight off infections and diseases, potentially aiding the body in combating cancer cells.
- Reduced Inflammation: Fasting has the potential to reduce inflammation in the body, which is a key factor in many chronic diseases, including cancer.
- Immune Cell Regeneration: Fasting may promote the regeneration of new immune cells, improving the overall immune response to cancer cells.
- Immune System Reset: Fasting could act as a reset for the immune system, helping to eliminate damaged or dysfunctional immune cells and replacing them with new, healthy ones.
Understanding how fasting impacts immune function is crucial in exploring its potential as an adjunct therapy in cancer treatment.
Combining Fasting With Other Therapies

Combining fasting with other therapies in cancer treatment can offer a synergistic approach that targets cancer cells from multiple angles. Dietary interventions play a crucial role in cancer therapy, and when fasting is combined with specific diets, it can enhance the effectiveness of treatment. Nutritional support during fasting periods is essential to ensure that the body receives adequate nutrients to maintain its functions while supporting the anti-cancer mechanisms.
Studies have shown that combining fasting with chemotherapy or radiation therapy can lead to improved treatment outcomes. Fasting may help sensitize cancer cells to these conventional treatments, making them more susceptible to the therapy's effects.
Additionally, fasting has been found to reduce the side effects associated with chemotherapy and radiation, thus improving the overall quality of life for cancer patients undergoing treatment.
Future Research Directions
Moving forward in the realm of cancer treatment research, an area that warrants exploration is the potential of fasting in combination with emerging immunotherapy strategies. This approach holds promise in enhancing the body's immune response against cancer cells. As researchers delve into this promising avenue, several key areas merit attention:
- Long term effects: Understanding how fasting, when integrated with immunotherapy, impacts patients' long-term outcomes and quality of life.
- Genetic implications: Investigating the genetic mechanisms underlying the synergistic effects of fasting and immunotherapy on cancer cells.
- Tumor microenvironment: Exploring how fasting may alter the tumor microenvironment to make it more susceptible to immunotherapy interventions.
- Personalized approaches: Developing personalized fasting regimens tailored to individual patients based on genetic profiles and specific cancer types.
Frequently Asked Questions
Can Fasting Be Harmful for Cancer Patients Undergoing Treatment?
Fasting can impact cancer patients undergoing treatment by potentially affecting their nutritional support and treatment compatibility. It's crucial to consult healthcare providers before fasting due to the risk of compromising therapy outcomes.
Some patients may benefit from modified fasting regimens, but individual circumstances vary. Balancing fasting benefits with treatment needs is essential for promoting overall well-being during cancer care.
Always prioritize open communication with your healthcare team when considering fasting.
What Types of Cancer May Benefit Most From Fasting?
Certain types of cancer, like breast cancer and pancreatic cancer, may benefit most from fasting. Studies suggest that fasting could potentially enhance the effectiveness of certain cancer treatments and reduce side effects. Fasting may help improve metabolic health, reduce inflammation, and increase the body's ability to combat cancer cells.
However, it's essential to consult with healthcare professionals before incorporating fasting into cancer treatment plans to ensure safety and effectiveness.
Is Intermittent Fasting as Effective as Prolonged Fasting for Cancer Prevention?
Intermittent fasting and prolonged fasting differ in duration and benefits for cancer prevention. While intermittent fasting involves shorter fasting periods, it still shows efficacy in reducing cancer risk.
Prolonged fasting, with its extended fasting periods, may offer more pronounced benefits. Both fasting methods have shown promise in cancer prevention, but the optimal approach may vary based on individual needs and health conditions.
Consulting with a healthcare provider is recommended for personalized guidance.
How Soon After Diagnosis Should Someone Start Fasting?
When pondering how soon to start fasting after diagnosis, remember that timing is key. The optimal timing varies for each individual. Consulting with healthcare professionals for an individualized approach is crucial.
Scientific evidence suggests that implementing fasting strategies tailored to personal needs and treatment plans could potentially enhance outcomes. Therefore, taking a data-driven approach to determine the best time to start fasting post-diagnosis is essential for maximizing potential benefits in cancer management.
Are There Specific Foods or Supplements to Avoid During Fasting for Cancer?
During fasting for cancer, it's crucial to maintain proper nutrient balance by avoiding high-sugar foods, processed meats, and excessive saturated fats. These choices can disrupt metabolic changes beneficial for treatment. Opt for whole foods rich in antioxidants, vitamins, and minerals.
Avoiding supplements unless advised by your healthcare provider is wise to ensure they don't interfere with treatment. Stay hydrated and focus on consuming a variety of nutrient-dense foods for optimal support during fasting.
Conclusion
In the battle against cancer, fasting emerges as a powerful ally, disrupting cancer cell metabolism and enhancing treatment effectiveness. Picture cancer cells weakened and vulnerable, while healthy cells thrive and regenerate. Harnessing the potential of fasting in combination with conventional therapies holds promise in improving outcomes for cancer patients. Further research is needed to unlock the full potential of fasting in the fight against cancer.